Nutrition Support Tips for ASD Kids with Constipation
Updated: March 1, 2024 · 10 Minute Read

Reviewed by:
May Zhu, Registered Dietitian at Begin Health
Highlights
- Kids with autism are often at higher risk of nutritional deficiencies due to their unique eating preferences
- Kids with ASD tend to consume diets low in fiber due to sensory issues, which can lead to problems with constipation
- Gastrointestinal symptoms are 4x more prevalent in children on the autism spectrum
- Incorporating prebiotic-rich foods can help not only increase overall fiber intake, but also boost probiotic function and support healthy digestion by increasing the overall amount of beneficial gut bacteria such as bifidobacteria
- Begin Health’s Growing Up Prebiotics can help bridge the fiber gap in autistic kids by providing 3g of tasteless and textureless prebiotic fiber per serving to help with softer stooling and improved gut health.
- Parents can help their kids promote regular bowel movements through consistent daily meal times, regular bathroom routines, daily exercise, and modeling healthy behaviors together
In the United States it is estimated that up to 95% of kids do not meet their daily recommended fiber intake.1 Children with Autism Spectrum Disorder (ASD) are 4x more likely to deal with gastrointestinal issues such as constipation and heartburn, compared to children without autism.2
Studies have shown children with autism are often at higher risk of nutritional deficiencies, metabolic imbalances, and gut problems due to their unique eating patterns. This is additionally exacerbated in kids with sensory processing disorders, who may have a limited diet as a result of adverse reactions to certain smells, tastes, and textures.3
Amidst the multifaceted nature of autism, dietary habits emerge as a significant contributor to constipation. The good news is that it’s also one of the factors that parents can help control to provide their little ones with relief. Let’s review the strategies for nutrition interventions and practical tips for parents to bridge the nutrition and fiber gap and prevent constipation in kids on the spectrum.
Nutrient Deficiencies in Kids with Autism
There are several factors as to why autistic kids struggle with eating but sensory issues remain as one of the most common reasons. Selective eating occurs when a kid consumes a very limited number of foods due to individual preferences in food texture, taste, colors, or shapes.
While selective eating can look different in each kid, a limited diet can lead to a lower intake of nutrients. Studies4 analyzing components of autistic children’s blood and tissue reveals they have lower levels of important nutrients, such as:
- Vitamins B3, B6, B12
- Vitamin C
- Vitamin D
- Calcium
- Iron
- Magnesium
- Zinc
Managing our little one’s diet to ensure our kiddos have the required amounts of each of these vitamins can go a long way in supporting overall development and preventing health deterioration.
Understanding the Fiber Gap in Autistic Children
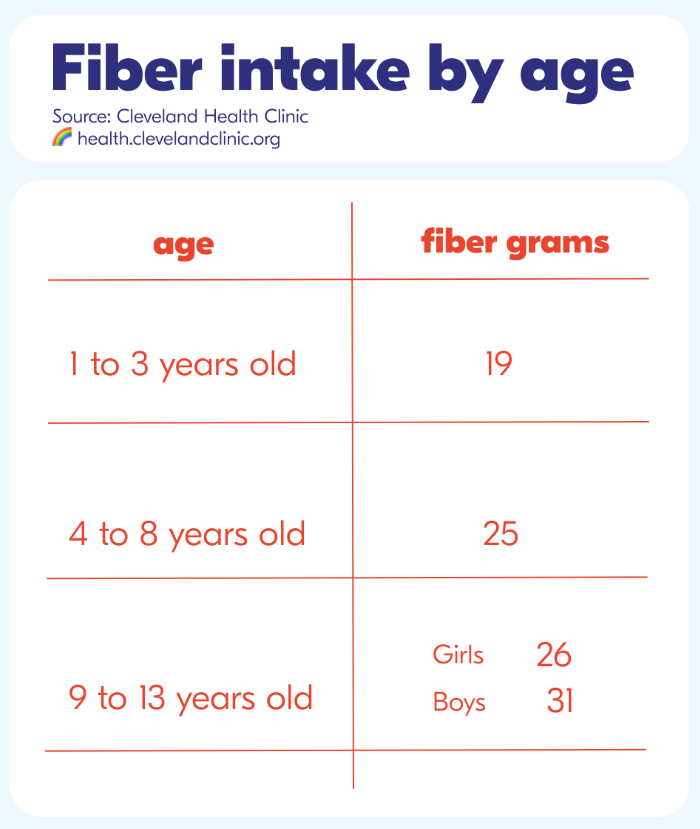
Research indicates that kids with ASD tend to consume diets low in fiber, contributing to constipation issues.5 Fiber plays a crucial role in maintaining bowel regularity by promoting bulk formation and stool softening.6 Addressing the fiber gap through dietary modifications is essential for managing constipation in ASD kiddos. The following chart shows the daily recommended amount of fiber for kids:
4 Nutrition Tips for Constipation Support in ASD Kids
1. Increase Fiber Gradually
Starting with a gradual approach to fiber intake can help with not only the adjustment of taste preferences, but digestive tolerance. Begin with modest servings of fiber-rich foods and progressively amplify by increasing portions weekly over the span of two to three weeks. This can help your kid’s digestive system get adjusted to the increase in fiber consumption. Adding too much fiber too quickly can cause bloating, gas, or cramps. Kids should drink plenty of water as well through this process, which helps move fiber through the intestines. Aim for an increase of one to two cups of extra water on top of their usual fluid intake daily.
2. Incorporating Probiotic and Prebiotic-Rich Foods
Studies suggest that combining foods rich in prebiotics and probiotics can create a synergistic effect in promoting a balanced and flourishing gut microbiota. A healthy gut microbiota is the key to maintaining good digestion. Prebiotics are a type of plant fiber that acts as the nourishment for probiotics, the live good type of bacteria in the digestive system. This synergistic effect enhances probiotic survival and activity in the microbiome. Both probiotics and prebiotics help foster an environment helpful to the growth of beneficial gut bacteria such a bifidobacteria, supporting digestion and overall gut health.7 Natural sources of prebiotic fiber include:
- Apples
- Bananas
- Carrots
Data from research also suggests that both prebiotics and probiotics may help alleviate common digestive issues such as constipation and diarrhea, creating a balanced environment in the gastrointestinal tract.8 Sources of probiotics include:
- Yogurt with live and active cultures
- Kefir
- Fermented foods such as kimchi, pickles or tofu
3. Sneak in Fiber
Fiber rich fruits and vegetables can be seamlessly integrated into your kid’s diets by blending into smoothies or soups to change the texture and tastes. Try pairing different fruits and vegetables with foods your little ones already know and love for them to get familiar with new choices.
For our extra picky eaters, a textureless and tasteless prebiotic fiber supplement such as Begin Health’s Growing Up Prebiotics can be a great option to add to their water or favorite beverage as an easy way to sneak in more fiber throughout the day. Studies show that prebiotic fiber such as chicory root fiber can help with softer and more frequent stooling within six weeks of daily use.9
4. Meet Daily Hydration Needs
Adequate water intake plays a pivotal role in bowel regularity. Data from multiple studies reveal an association between lower fluid intake, dehydration, and the increased risk for constipation.10 In addition to fluid intake, hydration can also come from water-rich fruits and vegetables such as cucumbers, berries, or melons. The amount of water a kid needs to drink every day can change based on activities and the food that they eat. It’s best to adjust based on your little one’s thirst cues.
Clear, pale yellow colored urine is a good sign that your little ones are drinking enough water. Darker, tea colored urine usually indicates the need to increase fluid consumption throughout the day.
Again, it is particularly important to increase your kid’s fluid intake when increasing fiber intake. Fluids will help soften the stool and make it easier to pass. While water is always the best option, certain juices (pear, apple or prune) can provide a natural laxative effect. Fluids that contain a lot of sugar or caffeine can make constipation worse - therefore it’s best to avoid or limit those options. A few more tips to help your kiddo increase fluid intake:
- Provide water in-between meal times, so your kiddos will not feel full before eating.
- Give water or water-rich fruits such as grapes, oranges or watermelon as a snack before physical activities.
- Keep a designated bottle or cup of water handy for your little ones to take sips anytime. Adding a wedge of citrus fruit like lemon or oranges to water can help give it more flavor.
- Model good behavior by setting the example. Kids are more likely to drink water when they see their parents and siblings drinking water too.
4 Lifestyle Tips for Kids with Constipation from an RD
1. Establish a Mealtime and Bathroom Routine.
Consistency through routine can help promote bowel regularity and establish healthy habits. Eating is a natural stimulant for the bowels, so developing a regular meal time daily can help kids develop consistent bowel movements.
2. Encourage Physical Activity.
Studies show that engaging in regular physical activity helps stimulate bowel movements to reduce the risk of constipation in kids.9 This can be as simple as playing catch outside, walking, or riding bikes. The American Heart Association recommends at least 60 minutes of moderate to vigorous physical activity daily for kids ages 6 years and up.
3. Create a Nurturing Mealtime Environment.
Studies show that stress can contribute to digestive problems due to the brain-gut connection.11 A stressful environment can also impact the way kids feel about certain foods. It’s critical to assess the mealtime environment in your home and make choices that help cultivate a stress-free atmosphere during mealtimes. This helps foster a nurturing environment free of stressors that may promote food aversions or digestive distress.
4. Model Healthy Nutrition Behaviors through Family Participation.
Children with autism who interact by assisting with the preparation of a food item may be more likely to attempt to taste that item. Activities such as cutting an apple, washing grapes, or adding toast to the oven may encourage your kids to eventually sample one of these items. Create a sense of empowerment within your little ones by involving them in meal planning and preparation to help them learn healthy behaviors with you and the rest of the family.
Your kids may feel that cooking something with you is just a fun activity. However, getting your little one to read the recipe and follow it will also assist with developing their academic skills in a natural environment. Not only can it expand reading skills, but it can also enhance their math skills. They can use their abilities to count, and measure in an enjoyable, stress-free environment.
Final Thoughts
The journey to bridging the fiber gap for ASD children with constipation will require a multifaceted approach that incorporates nutrition and lifestyle changes along with patience and persistence. Dietary modifications require time and consistency. Celebrating small victories is crucial as your family takes on this nutrition journey to creating a foundation of good health in your little ones. Parents who are looking to support a healthier gut environment in their kids can first address the fiber gap through diet choices by prioritizing prebiotic-rich foods, which can help with digestive balance.
Get our best articles delivered to your inbox each month.
We respect your privacy.
Article References
[1] Pashankar DS. Childhood constipation: evaluation and management. Clin Colon Rectal Surg. 2005 May;18(2):120-7. doi: 10.1055/s-2005-870894. PMID: 20011352; PMCID: PMC2780136.
[2] Fu SC, Lee CH, Wang H. Exploring the Association of Autism Spectrum Disorders and Constipation through Analysis of the Gut Microbiome. Int J Environ Res Public Health. 2021 Jan 14;18(2):667. doi: 10.3390/ijerph18020667. PMID: 33466802; PMCID: PMC7830459.
[3] Al-Beltagi M, Saeed NK, Bediwy AS, Elbeltagi R, Alhawamdeh R. Role of gastrointestinal health in managing children with autism spectrum disorder. World J Clin Pediatr. 2023 Sep 9;12(4):171-196. doi: 10.5409/wjcp.v12.i4.171. PMID: 37753490; PMCID: PMC10518744.
[4] Adams JB, Audhya T, McDonough-Means S, Rubin RA, Quig D, Geis E, Gehn E, Loresto M, Mitchell J, Atwood S, Barnhouse S, Lee W. Nutritional and metabolic status of children with autism vs. neurotypical children, and the association with autism severity. Nutr Metab (Lond). 2011 Jun 8;8(1):34. doi: 10.1186/1743-7075-8-34. PMID: 21651783; PMCID: PMC3135510.
[5] Gorrindo P, Williams KC, Lee EB, Walker LS, McGrew SG, Levitt P. Gastrointestinal dysfunction in autism: parental report, clinical evaluation, and associated factors. Autism Res. 2012 Apr;5(2):101-8. doi: 10.1002/aur.237. PMID: 22511450; PMCID: PMC3335766.
[6] Yang J, Wang HP, Zhou L, Xu CF. Effect of dietary fiber on constipation: a meta analysis. World J Gastroenterol. 2012 Dec 28;18(48):7378-83. doi: 10.3748/wjg.v18.i48.7378. PMID: 23326148; PMCID: PMC3544045.
[7] Markowiak P, Śliżewska K. Effects of Probiotics, Prebiotics, and Synbiotics on Human Health. Nutrients. 2017 Sep 15;9(9):1021. doi: 10.3390/nu9091021. PMID: 28914794; PMCID: PMC5622781.
[8] Closa-Monasterolo R, Ferré N, Castillejo-DeVillasante G, Luque V, Gispert-Llaurado M, Zaragoza-Jordana M, Theis S, Escribano J. The use of inulin-type fructans improves stool consistency in constipated children. A randomised clinical trial: pilot study. Int J Food Sci Nutr. 2017 Aug;68(5):587-594. doi: 10.1080/09637486.2016.1263605. Epub 2016 Dec 8. PMID: 27931142.
[9] Seidenfaden S, Ormarsson OT, Lund SH, Bjornsson ES. Physical activity may decrease the likelihood of children developing constipation. Acta Paediatr. 2018 Jan;107(1):151-155. doi: 10.1111/apa.14067. Epub 2017 Sep 27. PMID: 28898506.
[10] Konturek PC, Brzozowski T, Konturek SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options. J Physiol Pharmacol. 2011 Dec;62(6):591-9. PMID: 22314561.
[11] Boilesen SN, Tahan S, Dias FC, Melli LCFL, de Morais MB. Water and fluid intake in the prevention and treatment of functional constipation in children and adolescents: is there evidence? J Pediatr (Rio J). 2017 Jul-Aug;93(4):320-327. doi: 10.1016/j.jped.2017.01.005. Epub 2017 Apr 25. PMID: 28450053.













