How to get an autistic child to sleep: 15 tips
Updated: September 8, 2023 · 14 Minute Read

Reviewed by:
Amy Gong, Neurodiversity Advocate
Highlights
- Slightly adjust your child’s sleeping environment by lowering the temperature a few degrees, using a fan as white noise, or adding a weighted blanket to see if their sleep improves.
- Every child is different, but a good rule of thumb is to limit the activities they find stimulating for at least an hour before bedtime. Start non-stimulating activities before bed like light stretching or reading a book together.
- Many autistic children appreciate a consistent and predictable routine. Use a picture schedule to show children what to expect visually.
- Try to reduce your child’s exposure to blue light from cell phones, TVs, and tablets before bed while introducing plenty of sunshine during the day.
- Try offering your child their preferred snacks before bed in case they are hungry. Reduce foods that have caffeine or sugar like chocolate, peanut butter, juice, and milk.
- Try a melatonin or magnesium supplement. Add melatonin or magnesium-rich foods like milk, grapes (with the skin), beans, legumes/oats/rice, medicinal herbs, and pistachio nuts (or walnuts) to your child’s diet.
How to get an autistic child to sleep is one of the most common questions autism parents ask. Between 44% and 83% of kids on the spectrum have difficulty sleeping that affects their daily functioning.1 Many autistic people experience sleep disturbances such as early waking, nighttime awakenings, and irregular sleep patterns their whole lives.1
We understand how frustrating it can be when your child can’t sleep, so we’ve compiled the top tips from our autism sleep expert, the latest scientific research, and neurodiverse families. You can use these expert tips to help your child get a great night’s sleep – tonight!
How to get an autistic child to sleep: 15 tips
1. Take a sensory-friendly approach to your child’s sleeping environment by adjusting temperature, light, sound, textures, and smells.
Your child’s preferred sleeping environment might change from season to season. It might take some time to perfect your child’s sleeping environment. For sensory-sensitive children, the bedtime environment can make-or-break a good night’s sleep. You’ll want to go over their sleep environment with a fine tooth comb. Is the temperature right? (Lowering the temp before bedtime promotes sleep!) Are blankets, pillows, and pajamas as comfortable as possible? Is their room too bright or the decor (paint colors, decorations, etc.) too stimulating? Can they hear the washing machine or the drip of a faucet? Do they sleep better with white noise in the background? Try a fan or white noise fan to see if their sleep improves. Really be sure to see their room and surroundings from their perspective, and adjust accordingly. Sometimes it can be the little changes that make all the difference!
2. Create a consistent bedtime routine by spending time with your child doing non-stimulating activities before bed.
A successful bedtime routine will be consistent, predictable, and will include connection (focused one-on-one time) with you along with non-stimulating activities (such as a massage or reading a book). Every child is different, but a good rule of thumb is to limit the activities they find stimulating for at least an hour before bedtime. Choosing the right bedtime and wake time for your child, and keeping the same every day, is a crucial part of creating a good bedtime routine. It’s best to keep your child’s bedtime routine primarily in their room so that they do not form an association between sleep and you, or your room, or other rooms in the house, which could hinder their ability to sleep independently. Many autistic people take comfort in routine, so repeating the same process every night may help your child feel relaxed and prepared for sleep.
3. Use a picture schedule for your child’s bedtime routine.
For some kiddos, especially nonspeaking (nonverbal) kids on the spectrum, a schedule made from pictures that visually depict the bedtime routine can be a helpful tool. Many autistic children struggle with transitioning, so having a clear explanation of what to expect, and keeping that consistent, may ease anxiety and reduce uncertainty. If you find that your child has difficulty sticking to a bedtime routine, allowing them to choose the order the bedtime routine is completed in may be helpful. Your child can gesture to the activity they want to complete, and in what order, allowing them a sense of independence. Many autism families find that visual aids like this are a lifesaver for completing everyday activities.
4. Spend more time in the sun during the day and less time on the phone at night.
We know that exposure to blue light from cell phones, TVs, tablets, and computers can make sleeping difficult, but what about other forms of light? How do they affect sleep? Well, our bodies need exposure to daylight in order to regulate circadian rhythms that affect sleep. Your child’s body needs light during the day to signal to be awake, and dark during nighttime to stimulate sleep. Without the separation of dark and light, circadian rhythms can be disrupted and your child’s body may be “confused” about when it’s time to sleep and when it’s time to wake. Long story short, try to reduce your child’s exposure to blue light before bed while introducing plenty of sunshine during the day!
5. Eliminate or reduce sugar and caffeine in your child’s diet.
Cutting out soda and sweets in your child’s diet may be something you’re already doing, but did you know caffeine and sugar can hide in even the most inconspicuous foods? Chocolate, even some dark chocolate varieties, often contain caffeine, and sugar can be found in things like peanut butter, juice, and milk. They can stay in your child’s body for a while and make sleep difficult, so be sure to check food and beverage labels for sneaky caffeine and sugar content. If you do let your kiddo indulge, just make sure it’s early in the day so it has time to process out of their body before bedtime.
6. Make sure your child isn’t hungry by offering preferred snacks before bed.
Many autistic kids have difficulty recognizing or communicating when they’re hungry. As much as we try to ensure they’re getting enough to eat, even the most vigilant parents can still miss signs of hunger. Try offering your child snacks after dinner and before bed, or keep food visible and within their reach. Growth spurts and changes in environment or activity level may make your child hungrier than usual, making hunger easy to overlook as a possibility. Most kids can’t sleep when they’re hungry, and instead, some may “act out” with destructive behavior. If your child is just not going to sleep no matter what you do, or waking up frequently during the night, try offering them food. They may just be hungry!
Signs your child could be hungry (a lot of these are also signs your child may be sleepy! Often, the two sensations overlap):
- Destructive behavior such as throwing things, climbing on things, breaking things on purpose, when there is not a clear reason for the behavior change
- Aggressive behavior such as extra-rough play for seemingly no reason
- Pointing to or looking at foods (for example, staring at you while you’re eating a snack)
- Vocalizations or being extra frustrated (screaming, yelling, etc.)
- Not following directions as well as they normally would, even if they were just fine a moment ago
- Rejecting activities or just plain rejecting everything
- Frequent laying down and getting back up at bedtime
- Self-injury such as hitting themselves or banging against walls/doors
- “Foraging” for food such as searching through cabinets, going through empty containers/garbage, grabbing their lunch box (or for example, an old pizza box), opening refrigerator or pantry doors (and possibly throwing things out of them). This can look like being destructive or messy, but it may actually be your child expressing hunger.
- “Hoarding” food; this is especially common in kids who come from food scarcity or have suffered trauma in the past. The child may set aside food by their bed, under furniture, or in bed with them, or hide food throughout the house to save it for “later”. If your child is stashing bits of their dinner or lunch away, it could be because they’re getting hungry at night. Keep food available and visible to them all the time to ease their fears.
- Chewing on non-food objects or putting things in their mouth they know aren’t food.
- Bringing you a plate, utensil, or something related to food/eating. (For example, bringing you a spoon may seem random, but it could be your child’s way of expressing hunger.)
If your child doesn’t eat while at school or daycare and waits until they get home to eat, or if they don’t have consistent meal times, you’ll want to keep an extra eye out for signs of hunger.
Keep in mind that people with autism may become so overwhelmed by the sensation of hunger that they can’t eat. Their senses might be already overloaded, so sitting down or eating at that moment may feel like an even more overwhelming task. If you suspect your child may be hungry, but they’re rejecting everything you put in front of them, it’s probably because they’re too hungry. Of course, it’s best to cut off hunger before it gets to this “point of no return”, but if you can’t catch it in time, here’s an example of how to recover:
If your child is playing on the tablet, totally distracted and won’t eat, but you are pretty sure they’re hungry, it’s likely that they are past the hunger point and now can’t focus enough to eat. They’re focusing on their preferred activity (in this case, the tablet) in order to help them feel better. Try decreasing the amount of sensory input going on around your child (turning off technology, lowering/turning off lights, etc.), then set your child’s food where they normally eat (kitchen table, high chair, whatever), and move the tablet (or preferred activity) to where the food is.
7. Dedicate time for your child’s movement and play every day.
This is one tip that seems like an obvious thing but makes a world of difference! Now, if you’re like most autism parents we know, you’d probably say your child moves plenty during the day – in fact, sometimes it seems like they never stop moving! We hear you. However, creating pockets of time throughout the day where your child can participate in purposeful, focused movement, and burn off energy is crucial to a restful night. It also makes it easier for kids to focus on tasks and participate in school, therapy, at home, etc. You’ll find that plenty of purposeful movement produces a much calmer kid. This could be time at the playground or in the backyard, movement games, yoga, jumping jacks, races from one end of the hall to the other – any kind of physical, prolonged movement that will get their heart pumping and expel all that energy.
8. Try adding light exercise like stretching or yoga to your child’s bedtime routine.
Many sleep experts used to recommend not engaging in exercise before bed, but newer research suggests movement before bed can actually help people with insomnia fall asleep faster and sleep deeper.5 So, if you find that your child is restless toward the end of the day, or if your child struggles with insomnia (the inability to fall asleep), try adding some light exercise to their bedtime routine. Of course, you’ll want to avoid any strenuous activity for at least an hour before bed; but stretching, yoga, pilates, or a walk/stroller ride around the neighborhood, are all great options for light activity that gets their energy out without raising their heart rate too much.
9. Make sure your child uses the bathroom before bed.
It may seem like a simple tip, but it’s an often overlooked one. Many children with autism experience gastrointestinal issues like constipation, so using the bathroom (number one and two!) before going to bed can prevent nighttime awakenings associated with tummy discomfort. If your child has difficulty using the restroom or having bowel movements, check with their doctor about appropriate supplements and diet changes that can help them get regular. If your child is still in diapers or pull-ups, give them a fresh one before they fall asleep to ensure a more comfortable rest. (I can’t tell you how many times my son has woken up due to a wet pull-up.)
10. Try a melatonin supplement.
Experts suspect that sleep issues in autistic people may stem from a lack of production of neurotransmitters that regulate sleep.1,2 For some parents (like us), a children’s melatonin supplement is a lifesaver. (We like Natrol liquid or fast dissolve tablets in 1mg, or Spring Valley gummies in 1mg the best.)
Be sure to read the label on melatonin products because manufacturers all have differing ways of dispersing the melatonin throughout the product. For example, it takes 4 full droppers of Natrol liquid melatonin to equal 1mg. A lot of melatonin supplement manufacturers also add in additional ingredients to promote sleep like lavender, but we’ve found that those don’t work so great for our kids. (Every child is different).
When figuring how much to dose, less is more, because dosing too much melatonin can create a counter effect (your child up all night). It’s also important when you dose. If you give your child melatonin too early before they’re ready to sleep, you run the risk of them becoming grumpy and tired but unable to sleep. Dose too late and you may encounter what I call a “baby-nado” (baby tornado), that is, a wide awake but grumpy and destructive kiddo.
We recommend starting off your child with half of 1mg when you see signs they may be sleepy, but before they “hit the wall”. Look for tired eyes, rubbing eyes, laying down (even if it’s just briefly), or seeming less interested in play or preferred activities. If it doesn’t help them fall asleep, try the full 1mg next time. This is the method that worked for us, but check with your child’s doctor before beginning any supplements and for dosing recommendations based on your child’s weight and age.
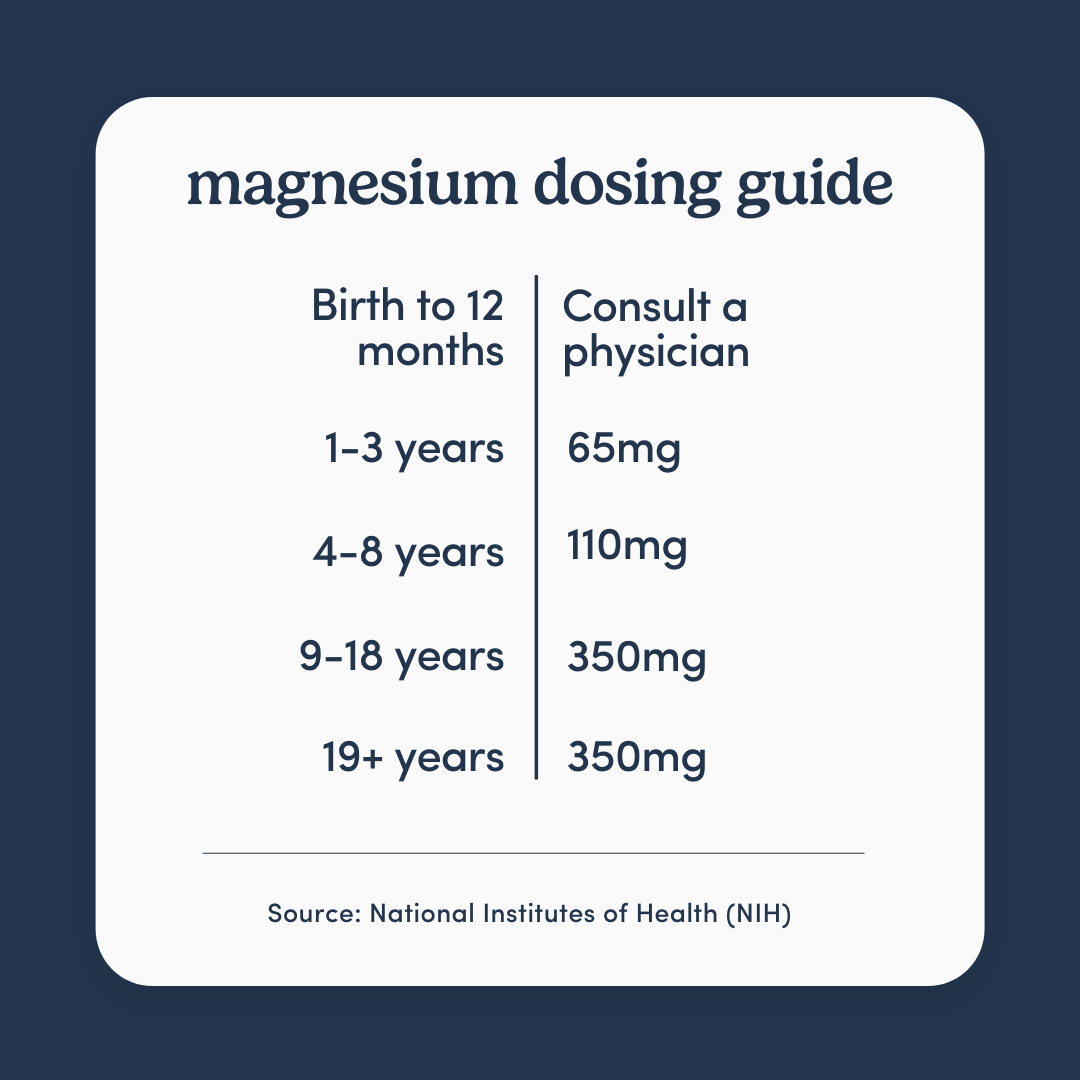
11. Try a magnesium supplement.
If you are looking for a supplement that causes little to no side effects, magnesium has recently become a popular supplement to help improve sleep. Magnesium is an important mineral responsible for over 300 processes in the body (sleep is one of them)! 1 in 2 Americans do not get enough magnesium daily which means many people need a combination of magnesium rich foods (cashews, almonds, peas, and beans) and supplements to get enough magnesium in their diet.7 Teenagers and people with gastrointestinal disorders are at higher risk for insufficient magnesium levels.8
Similar to our melatonin tip, you should check with your child’s doctor before beginning any supplements and for dosing recommendations based on your child’s weight and age. Popular types of magnesium supplements include powder, gummies, and oil. Some parents we interviewed recommend putting magnesium lotion on the belly or feet!
Holistic additions to your child’s night time routine:
Although there’s limited data to support these additions, parents may find that incorporating things like weighted blankets, music, or essential oils (via a massage or scent) can help their child rest. Our expert recommends trying melatonin first, with the input of your child’s physician, before trying these non-evidence-based methods.
12. Try a weighted blanket.
Some kids may find the compression from a weighted blanket to be relaxing. Although we don’t have data which shows the same for kids, weighted blankets have been shown to help adults with anxiety by forcing the autonomic nervous system into “rest” mode, promoting an overall sense of calm.3 If your child is restless, a weighted blanket may be a good option. Just remember to choose the appropriate weight so your child is able to breathe and rest comfortably. When choosing the right weight of blanket for your child, it should be easy for your child to take off or move on their own. Children under two, or those who lack the motor skills necessary to move the blanket themselves, should not use weighted blankets.
13. Play soothing music.
Music can be a valuable part of a child’s sleep training, providing a familiar and relaxing cue that it’s time to sleep. For autistic kiddos who may be sensitive to sound, white noise can “tune out” the irritating sounds around them that can disturb their sleep, giving them something else to focus on as they drift off. Your child may also enjoy a sensory-friendly bedtime video with calming music. (We like the lantern video from Hey Bear Sensory, or sea life videos like this.)
14. Add scent with essential oils.
Some children may find the scent of lavender, camomile, or other essential oils to be calming. You could also try using essential oils while giving your child a pressure massage on arms, legs, and back. Some parents swear by deep tissue massages for helping kids relax before bedtime. There are also essential-oil infused room or pillow sprays that can add a soothing scent to the room, which some believe promotes sleep. Always use caution when applying products to your child’s skin or spraying/dispersing fragrances nearby. Your child may be allergic or otherwise sensitive to certain scents and products.
15. Add melatonin-rich foods to your child’s diet.
This is another topic that has mixed research findings. However, one study does suggest that foods naturally high in melatonin may help our bodies produce more melatonin.6 You can try adding foods like milk, grapes (with the skin), beans, legumes/oats/rice, medicinal herbs, and pistachio nuts (or walnuts) to your child’s diet, and see if it helps them sleep better. For a long time, many people have sworn by cherries or cherry juice as a natural sleep aid, however, the data shows cherries have about the same amount of melatonin as strawberries, and slightly less than grapes with the skin. (Note that melatonin wasn’t found in juices or products from concentrate, only in whole fruits or fresh/bottled juice.)
Consult your child’s doctor to rule out medical causes for sleep disturbance.
Experts recommend ruling out any medical causes and trying a non-medicinal approach for your child’s sleep problems before resorting to medication. If you’ve tried everything to get your child to sleep and nothing has worked, a trip to the doctor may be in order. Studies have shown that doctors don’t always check autistic kids thoroughly for the cause of sleep disturbances due to many factors, so be sure to advocate for your child to get a thorough check, and keep advocating for answers.2 Your child’s doctor may recommend medication that can help your child sleep better if other methods aren’t working.
There’s more tips where these came from! If you’d like more expert-reviewed tips for getting your autistic child to sleep, check out our full sleep guide or sign up for our newsletter!
Get our best articles delivered to your inbox each month.
We respect your privacy.
Dive Deeper
Article References
- Williams Buckley A, Hirtz D, Oskoui M, et al. Practice guideline: Treatment for insomnia and disrupted sleep behavior in children and adolescents with autism spectrum disorder: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurology. 2020;94(9):392-404. doi:10.1212/WNL.0000000000009033
- Won, D., Feldman, H.M., Huffman, L.C. (2019). Sleep Problem Detection and Documentation in ChildrenWith Autism Spectrum Disorder and Attention-Deficit/Hyperactivity Disorder by Developmental-BehavioralPediatricians: A DBPNet Study. Journal of Developmental & Behavioral Pediatrics, 40:20–31
- Pennmedicine.org. Published 2022. Accessed August 31, 2022. https://www.pennmedicine.org/updates/blogs/health-and-wellness/2022/march/weighted-blankets#:~:text=The%20pressure%20of%20weighted%20blankets
- Myllymäki T, Kyröläinen H, Savolainen K, Hokka L, Jakonen R, Juuti T, Martinmäki K, Kaartinen J, Kinnunen ML, Rusko H. Effects of vigorous late-night exercise on sleep quality and cardiac autonomic activity. J Sleep Res. 2011 Mar;20(1 Pt 2):146-53. doi: 10.1111/j.1365-2869.2010.00874.x. PMID: 20673290.
- Does exercising at night affect sleep? Harvard Health. Published April 1, 2019. Accessed September 1, 2022. https://www.health.harvard.edu/staying-healthy/does-exercising-at-night-affect-sleep#:~:text=Traditionally%2C%20experts%20have%20recommended%20not
- Meng X, Li Y, Li S, et al. Dietary Sources and Bioactivities of Melatonin. Nutrients. 2017;9(4):367. Published 2017 Apr 7. doi:10.3390/nu9040367
- Summer, J. Using Magnesium for Better Sleep. Sleep Foundation. Published May 20, 2021. https://www.sleepfoundation.org/magnesium
- National Institute of Health Office of Dietary Supplements. Magnesium Fact Sheet for Professionals. osd.nih.gov. Published March 29, 2021. https://ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/













